Prostate cancer screening and the prostate-specific antigen (PSA) test
Patient information leaflet regarding PSA testing (Public Health England 2016)
At best, screening for prostate cancer leads to a small reduction in disease-specific mortality over 10 years but has does not affect overall mortality.
History relevant to requesting PSA test and/or undertaking digital rectal examination DRE
Are you symptomatic?
Symptomatic LUTS
Storage: frequency, urgency, nocturia
Voiding: hesitancy, poor stream, incomplete emptying, terminal dribbling, retentionErectile Dysfunction
Visible haematuria
Cancer symptoms: weight loss, back pain, bone pain, loss of appetite, lethargy
Do you have risk factors for prostate cancer?
Increasing age
Black ethnicity
Family history of prostate cancer
Obesity or being overweight
Prostate-specific antigen (PSA)
PSA is a protein produced by normal and cancerous prostate cells.
False-negative PSA tests (low sensitivity)
15% of men with a negative PSA test may have prostate cancer
False-positive PSA tests (low specificity)
75% of men with a positive PSA test have a negative prostate biopsy
Unnecessary treatment
A positive PSA test may lead to the identification and treatment of prostate cancers which would not have become clinically evident during the man’s lifetime
Causes of elevated PSA: prostate cancer, benign prostatic enlargement, prostatitis [vigorous exercise, ejaculation, UTI, recent prostate biopsy]
Causes of lowered PSA: obesity, 5 alpha-reductase inhibitors (e.g. finasteride), statins, thiazide diuretics
Abstain from ejaculation & vigorous exercise for 48hr prior to test, and ensure no UTI prior to test
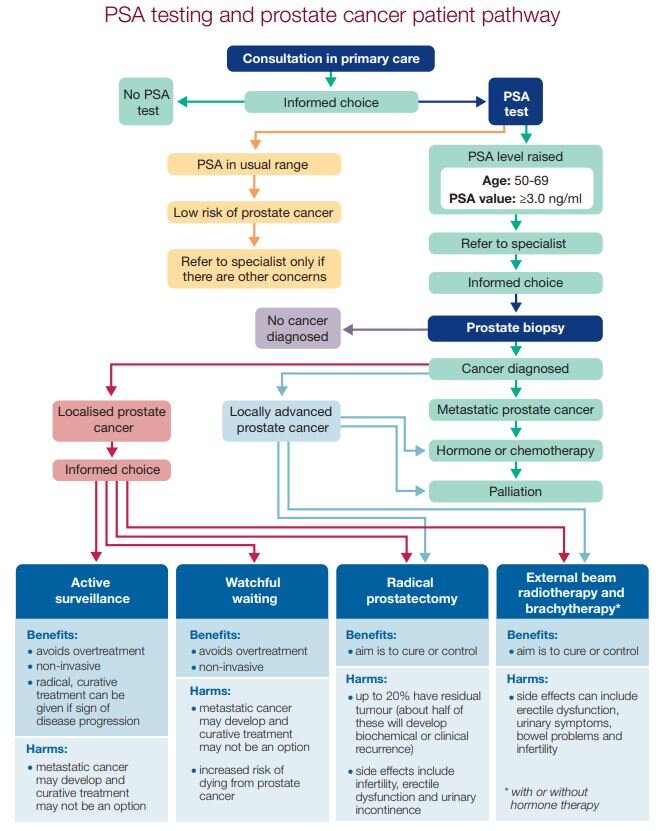
How should I interpret and manage PSA results?
Normal PSA range: 0–4 nanograms/mL.
Urgently (2ww) refer
if patient is aged 50–69 years and PSA >3 ng/mL OR prostate is hard and nodular on DRE
Consider referral
if PSA is within normal range AND clinical concerns (such as abnormal prostate on digital rectal examination (DRE) or suspicion of higher risk for prostate cancer)
Repeating PSA test?
4 years is suggested as the optimal interval for repeat testing
Recommendations may be affected in the future by changes to practice such as greater use of mp-MRI (multi-parameter MRI)
Prostate cancer
Lifetime risk 1 in 8 (1 in 4 for black men); 1 in 40 will die from prostate cancer
Almost all cancers of the prostate (95%) are adenocarcinomas: prostate cancer is multifocal
Diagnosis of prostate cancer (primary care setting):
A digital rectal examination (DRE)
A prostate-specific antigen (PSA) test
Definitive diagnosis requires a biopsy, often performed via guided imaging
Assessment
Prostate biopsy: TRUS biopsy (transrectal ultrasound-guided biopsy of the prostate: risk of FP (detects early low-grade cancers, not causing mortality) and FN (missing high-grade small tumours). Complications: haematuria, pain, fever, sepsis
MP-MRI Multiparametric MRI imaging of the prostate: better at detecting high-grade tumours
Treatment for prostate cancer
Active surveillance
Watchful waiting
Radical prostatectomy
External beam radiotherapy
Adjunctive hormonal treatment, or chemotherapy