Transient Ischaemic Attack (TIA)
Definition
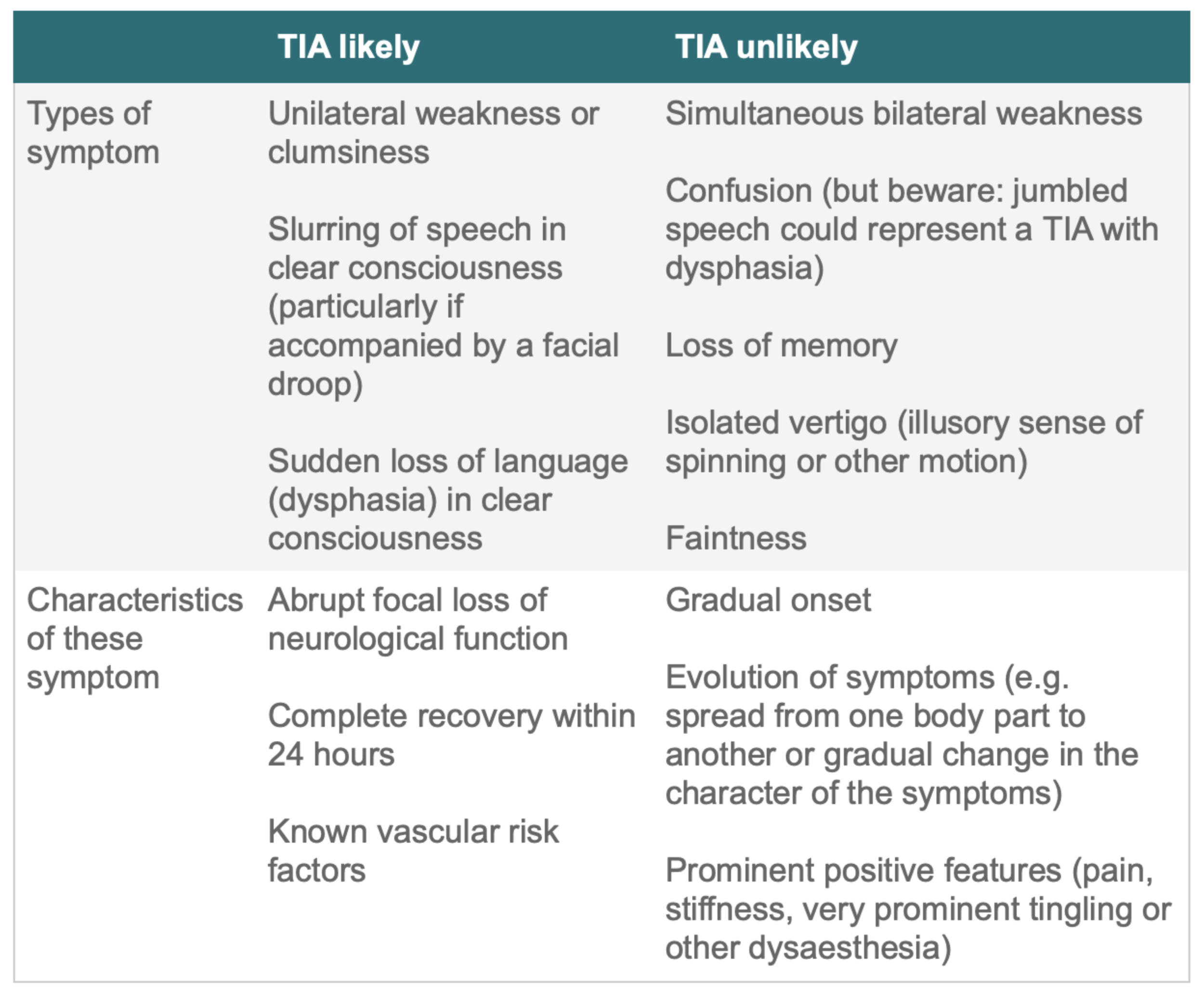
TIA should be suspected when a person presents with sudden onset, focal neurological deficit (causing brain, spinal cord or retinal ischaemia) which has completely resolved within 24 hours of onset. Most TIAs are thought to resolve within 1 or 2 hours but can persist for up to 24 hours
Once a person has had a stroke or TIA they are at high risk of a further vascular event.
Symptoms of TIA:
Unilateral weakness or sensory loss
Dysphasia
Ataxia, vertigo, or incoordination
Syncope
Sudden transient loss of vision in one eye (amaurosis fugax)
Homonymous hemianopia
Cranial nerve defects
Diagnosis of transient ischaemic attack (TIA)
Acute onset neurological symptoms:
Use a validated tool, such as FAST (Face Arm Speech Test) outside hospital OR ROSIER (Recognition of Stroke in the Emergency Room) in the emergency department.Exclude hypoglycaemia
Initial management of suspected and confifirmed TIA
Offer aspirin (300 mg daily), start immediately (see below for recommendation to commence DAPT)
Refer immediately (see within 24 hours of onset of symptoms) to a stroke unit/stroke physician
Do not use scoring systems, such as ABCD2, to assess risk of subsequent stroke or to inform urgency of referral for people who have had a suspected or confirmed TIA.
Investigations for TIA and secondary prevention
1.Brain imaging
Do not offer CT brain unless there is clinical suspicion of an alternative diagnosis that CT could detect.
Consider same day MRI (including diffusion-weighted and blood-sensitive sequences) to determine the territory of ischaemia, or to detect haemorrhage or alternative pathologies.
2. Assessing and managing carotid stenosis (carotid ultrasonography)
Offer carotid endarterectomy if carotid stenosis of 50 to 99% according to the NASCET (North American Symptomatic Carotid Endarterectomy Trial) criteri.
Not for carotid endarterectomy if carotid stenosis less than 50% (NASCET criteria) or less than 70% (European Carotid Surgery Trial ECST criteria).
Consider carotid artery stent stenting for people unable to have endarterectomy.
3. Cardioembolic source
Cardiac echocardiogram/transoesophageal echocardiography
imaging of the aorta (aortic atherothrombosis)
imaging of the left atrial appendage (left atrial clot)
Patent foramen ovale: percutaneous closure of patent foramen ovale to prevent recurrent cerebral embolic events
Atrial fibrillation (permanent and paroxysmal) : admission ECG, Ambulatory 24hr or 72hr ECG
4. Cardiovascular co-morbidities
Hypertension, diabetes, hypercholesterolaemia
Preventing further occlusive vascular events
1.ANTIPLATELET THERAPY
BMJ Clinical Practice Guideline, based upon a published BMJ Systematic review
Clopidogrel plus aspirin versus aspirin alone for acute minor ischaemic stroke or high risk transient ischaemic attack: systematic review and meta-analysis BMJ 2018;363:k5108
In patients who have experienced a high risk transient ischaemic attack or minor stroke, the guideline recommends dual antiplatelet therapy (DAPT) with clopidogrel and aspirin to be started within 24 hours , and continued for 10-21 days, and thereafter, continue with single antiplatelet therapy.
Start immediately: Aspirin daily 300 mg
Following confirmation of TIA by Stroke/TIA Clinic:
First-line: Aspirin daily 300 mg AND Clopidogrel (off-licence use)
Second-line: Aspirin AND Modified-release dipyridamole
Clopidogrel is licensed for the prevention of atherothrombotic events following myocardial infarction, ischaemic stroke or established peripheral arterial disease.
Proton pump inhibitor: if previous dyspepsia associated with aspirin is reported.
2.MANAGE CARDIOVASCULAR CO-MORBIDITIES
control of blood pressure
antiplatelet agents
diabetes
cholesterol lowering through diet and drugs
lifestyle advice