Red Eye
ANY unilateral red eye, reduced acuity, pain, photophobia, pupil abnormalities or trauma —> NEEDS URGENT REFERRAL
Serious and potentially sight-threatening causes of red eye include:
Acute glaucoma
Corneal ulcer, contact lens-related red eye and corneal foreign body.
Anterior uveitis
Scleritis
Trauma, such as penetrating eye injury or high-velocity foreign body
Chemical injuries
Neonatal conjunctivitis
ASSESSMENT
HISTORY
Onset and duration of symptoms
If symptoms are unilateral or bilateral
Associated symptoms: visual changes, pain, foreign body sensation, discharge, photophobia
Use of contact lenses
Any history of trauma, foreign body or chemical exposure
Any similar episodes in the past
Past medical history
hypertension
connective tissue disorders
anticoagulant use
eye drops
EXAMINATION
Inspection and checking for photophobia and eye pain/eye pain on eye movement
Unilateral red eye
Eye pain: mild (conjunctivitis ‘pink eye’, episcleritis); moderate-severe (corneal ulcer/foreign body, scleritis); orbital pain (anterior uveitis or glaucoma if sudden-onset orbital pain); pain on eye movement (optic neuritis due to MS or infection, scleritis, orbital cellulitis)
Photophobia: may indicate glaucoma, acute uveitis, corneal ulcer, contact lens-related red eye or corneal foreign body
Examine:
Sclera: widespread redness is most concerning, however, segmental could indicate subconjunctival haemorrhage or episcleritis
Cornea for any localised discolouration, ulceration or foreign body (re-check if any history of contact lens use)
Ciliary injection/flush (limbal vessels at junction of cornea and sclera) suggest corneal ulcer, contact lens related red eye, corneal foreign body and anterior uveitis
Conjunctiva, including the tarsal surface: if a foreign body is a possibility, the upper lid should be everted to check for a sub-tarsal foreign body.
Eye lids for discharge/sticky eyelids: which may signify blepharitis, conjunctivitis, trichiasis, entropion, ectropion or molluscum
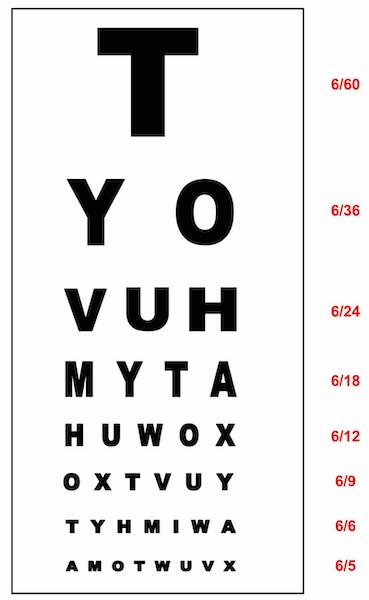
Assessment of visual acuity
Use Snellen Chart or LogMAR Chart and record acuity.
6/6 = normal vision, 6/12 minimum DVLA limit for driving, 6/5 better than normal vision
Pupil reactions
Check direct and consensual pupillary reflexes: elicited via direct light reaction, consensual light reaction or finger-to-nose convergence test
Mid-dilated pupil (acute glaucoma)
Constricted pupil with painful accommodation (anterior uveitis)
Fluorescein examination
Apply fluorescein drops (+ proxymetacaine LA) and illuminate with cobalt blue light
Cornea focally stains : traumatic corneal abrasion or ulcer or foreign body or dendritic ulcers (HSV)
Special considerations
Trauma: if perforation of the globe is suspected (for instance in ocular trauma or as a complication of scleritis), do not palpate the eye - arrange for urgent ophthalmology assessment.
Check for hypertension and clotting abnormalities if subconjunctival haemorrhage is suspected
MANAGEMENT
REFER FOR SAME-DAY OPHTHALMOLOGIST ASSESSMENT (suspected serious, and potentially sight-threatening)
Unilateral red eye
Deep pain within the eye
Photophobia
Reduced visual acuity
High-velocity injury
Chemical eye injury
Ciliary injection
Fluorescein staining of the cornea
Unequal or misshapen pupils or abnormal pupillary reactions
Painful pupillary constriction
Contact lens use
Red, sticky eye in an infant in the first 28 days of life
BENIGN CONDITIONS NOT REQUIRING OPHTHALMOLOGIST REFERRAL
Blepharitis inflammation of the eyelids, gritty eye sensation, symmetrical and bilateral.
Associated with dysfunction of the meibomian gland or staphylococcal hypersensitivity.
There is no discharge, although there may be crusting in the mornings.
Treatment is with topical lubricants and lid hygiene, involving hot compresses and scrubbing the bases of the eyelashes with cotton wool buds dipped into hot water and baby shampoo.Conjunctivitis- infective: bilateral discharge that can be watery/serous, recent URTI (viral, ‘pink eye’); mucous (chlamydial); copious, purulent, sticky eyelashes (bacterial gonococcal)
Conjunctivitis- allergic: bilateral, itchy, discharge worse in morning, seasonal, history of atopyDry eye syndrome (no discharge, gritty or burning feeling)
Subconjunctival haemorrhage.
This is due to a bleed into the subconjunctival space. Often painless. Not associated with corneal opacity.
There may ocontributory factors: straining with coughing or constipation, hypertension or anticoagulant use.
On examination, there is an area of localised, well-demarcated haemorrhage in one eye, in the absence of pain, no reduction of visual acuity, normal pupil reactions, and no corneal staining. Reassure the person that the haemhorrage will clear in 2 weeks.
Refer to ophthalmology if subconjunctival haemorrhage AND head injury AND you cannot see the posterior aspect of the haematoma laterally, as this may indicate a base of skull fracture.Episcleritis
This presents with segmental redness and low-grade pain in one or both eyes.
On examination, there is segmental redness, with normal vision, pupil reactions, and no corneal staining.
Episcleritis is usually self-limiting (2 weeks). Consider oral NSAIDs to aid recovery.Ectropion, entropion and trichiasis.
Ectropion (outward rotation of the eyelid margin).
Entropion (inward rotation of the eyelid margin).
Trichiasis (misdirection of the eyelashes towards the cornea).
Ectropion can cause exposure keratopathy, and entropion and trichiasis can cause corneal irritation and abrasion.
If there are no features which indicate a serious cause refer routinely to ophthalmology.
Surgical correction may be required.Subtarsal or conjunctival foreign body
Corneal superficial injury
Other conditions to be aware of
Herpes zoster ophthalmicus
Reactivation of varicella zoster virus infection in the ophthalmic division of the trigeminal nerve.
It can be treated in the community.
But if the eye becomes red, then refer the patient to an ophthalmologist.
If the tip of the nose is uninvolved, intraocular involvement is unlikely.
Treatment is with oral valaciclovir.