Constipation in children
CKS Constipation in children
NICE patient information: Constipation in children and young people
Definition
Constipation is a decrease in the frequency of bowel movements (<3 stools weekly since birth)
characterised by the passing of hardened stools which may be large and associated with straining and pain.
Constipation affects 5–30% of the child population, depending on the criteria used for diagnosis
Normal physiology
Stool frequency:
4 per day in the first week of life
2 per day at 1 year of age.
Frequency of stool ranges from 3 per week TO 3 stools per day ; this range is usually attained by 4 years of age.
Diagnosis
Constipation is termed idiopathic (functional) if it cannot be explained by any anatomical or physiological abnormality.
Faecal impaction:
A history of severe symptoms of constipation
Overflow soiling
A faecal mass palpable on abdominal examination
Constipation:
Infrequent bowel activity (<3/week) unless exclusively breastfed
Hard, large stool
'Rabbit droppings' stool
Overflow soiling very loose, smelly stools, passed without sensation
Risk factors
Pain (such as painful defecation)
Fever
Inadequate fluid intake
Reduced dietary fibre intake
Toilet training issues
Drug side-effects
Psychosocial issues
Family history of constipation
Cerebral palsy
Down's syndrome
Autism
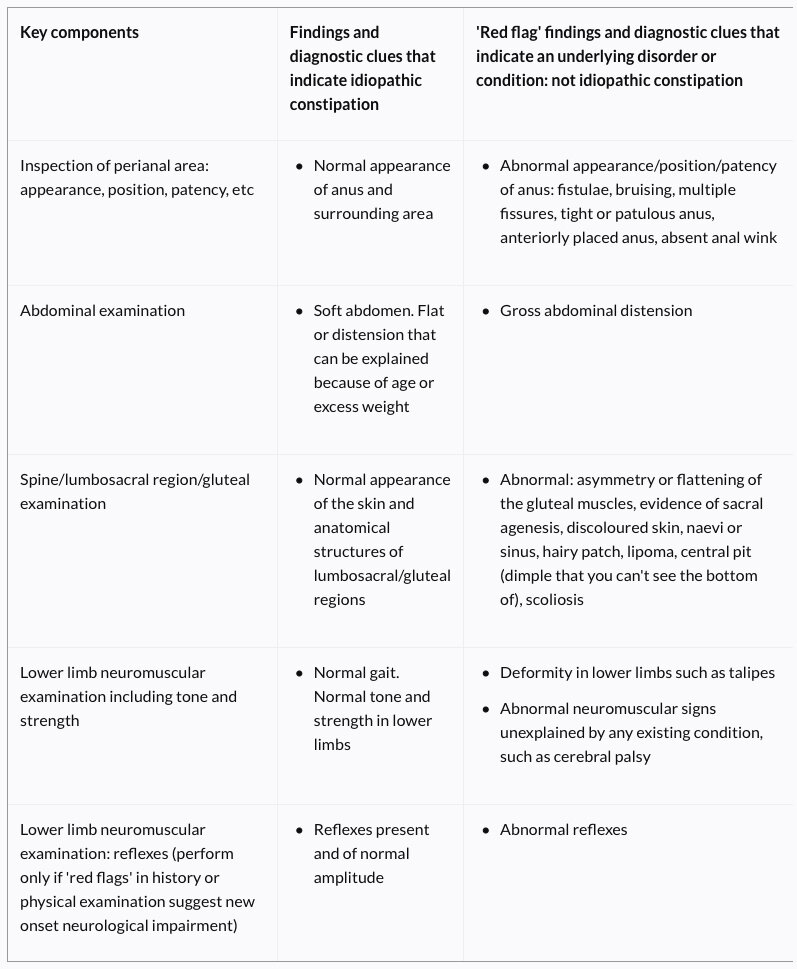
Red flags: refer the child urgently, do not initiate treatment for constipation in primary care
Timing of onset of constipation and potential precipitating factors: reported from birth or first few weeks of life
Failure to pass meconium/delay (>48h after birth in term baby)
'Ribbon stools' (more likely in a child younger than 1 year)
Faltering growth and/or weight loss
Previously unknown or undiagnosed weakness in legs, locomotor delay
Abdominal distension with vomiting
Abnormal appearance/position/patency of anus: fistulae, bruising, multiple fissures, tight or patulous anus, anteriorly placed anus, absent anal wink
Gross abdominal distension
Abnormal: asymmetry or flattening of the gluteal muscles, evidence of sacral agenesis, discoloured skin, naevi or sinus, hairy patch, lipoma, central pit (dimple that you can't see the bottom of), scoliosis
Deformity in lower limbs such as talipes
Abnormal neuromuscular signs unexplained by any existing condition, such as cerebral palsy
Lower limb neuromuscular examination: abnormal reflexes
Amber flags- also require specialist referral for assessment, but treatment for constipation may be initiated in primary care whilst awaiting specialist assessment
Evidence of faltering growth, developmental delay, or concerns about wellbeing.
Constipation triggered by the introduction of cows' milk.
Concern of possible child maltreatment.
Investigations
If requested by specialist services, consider testing for
coeliac disease
hypothyroidism
cystic fibrosis
electrolyte disturbance
cows' milk protein allergy
Digital rectal examination
A digital rectal examination should be undertaken only by healthcare professionals competent to interpret features of anatomical abnormalities or Hirschsprung's disease.
If a child younger than 1 year has a diagnosis of idiopathic constipation that does not respond to optimum treatment within 4 weeks, refer them urgently to a healthcare professional competent to perform a digital rectal examination and interpret features of anatomical abnormalities or Hirschsprung's disease.
Do not perform a digital rectal examination in children or young people older than 1 year with a 'red flag' —> refer them urgently to a healthcare professional competent to perform a digital rectal examination and interpret features of anatomical abnormalities or Hirschsprung's disease.
Management of idiopathic constipation (red and amber flags excluded)
Paediatric formula:
Oral powder: macrogol 3350 (polyethylene glycol 3350) 6.563 g; sodium bicarbonate 89.3 mg; sodium chloride 175.4 mg; potassium chloride 25.1 mg/sachet (unflavoured)
Maintenance laxatives if impaction is not present or has been successfully treated.
Child under 1 year: ½–1 sachet daily
Child 1–6 years: 1 sachet daily;(maximum 4 sachets daily)
Child 6–12 years: 2 sachets daily; (maximum 4 sachets daily)
Faecal impaction —> disimpaction laxative regimen
Child under 1 year: ½–1 sachet daily
Child 1–5 years: 2 sachets on 1st day, then 4 sachets daily for 2 days, then 6 sachets daily for 2 days, then 8 sachets daily
Child 5–12 years: 4 sachets on 1st day, then increased in steps of 2 sachets daily to maximum of 12 sachets daily
Add a stimulant laxative (sodium picosulfate, bisacodyl, Senna, docusate sodium) if macrogol 3350 does not work.
Add another laxative such as (osmotic laxative) lactulose or (stimulant laxative) docusate if stools are hard.
Diet
Adequate fluid intake
Adequate fibre. Recommend including foods with a high fibre content (such as fruit, vegetables, high-fibre bread, baked beans and wholegrain breakfast cereals)
Do not recommend unprocessed bran, which can cause bloating and flatulence and reduce the absorption of micronutrients.
Behavioural interventions
Scheduled toileting, use of a bowel habit diary, and reward systems.
Specialist referral
Considering the need for specialist referral if symptoms do not respond to optimal treatment in primary care, or if there is faecal impaction and the child is very distressed.
Refer children and young people with idiopathic constipation who do not respond to initial treatment within 3 months to a practitioner with expertise in the problem
Referral for specialist assessment by a paediatrician is indicated in constipation when:
An underlying cause is suspected
There are 'red flags' such as failure to thrive, distended abdomen, blood and/or mucus in the stools
Treatment is unsuccessful
Management is complex (and requires more than the advice, support, and prescription of laxatives that can be provided in primary care because there are major psychological causes or consequences)
Referral to a paediatric continence adviser/specialist nurse should be considered when there is soiling and/or faecal loading requiring disimpaction. It is also important to be alert to the rare possibility of child abuse.
Rectal medications
Do not use rectal medications for disimpaction unless all oral medications have failed and only if the child or young person and their family consent.
Administer sodium citrate enemas only if all oral medications for disimpaction have failed.