Alcohol-related liver disease ARLD
Background
Alcohol-related cirrhosis is the the most common cause of liver-related mortality in Western populations.
25% of the population drink more than recommended guidelines (≤14 units/week), with 10% drinking twice as much and 1.4% drinking more than 75 units/week.
The relationship between alcohol consumption and liver cirrhosis is exponential;
at 20 units/week the relative risk is approximately 3
at 80 units/week it is 30.1
There is also a synergy between alcohol intake and obesity;
when body mass index (BMI) is >35, the risk of liver disease doubles for any given alcohol intake
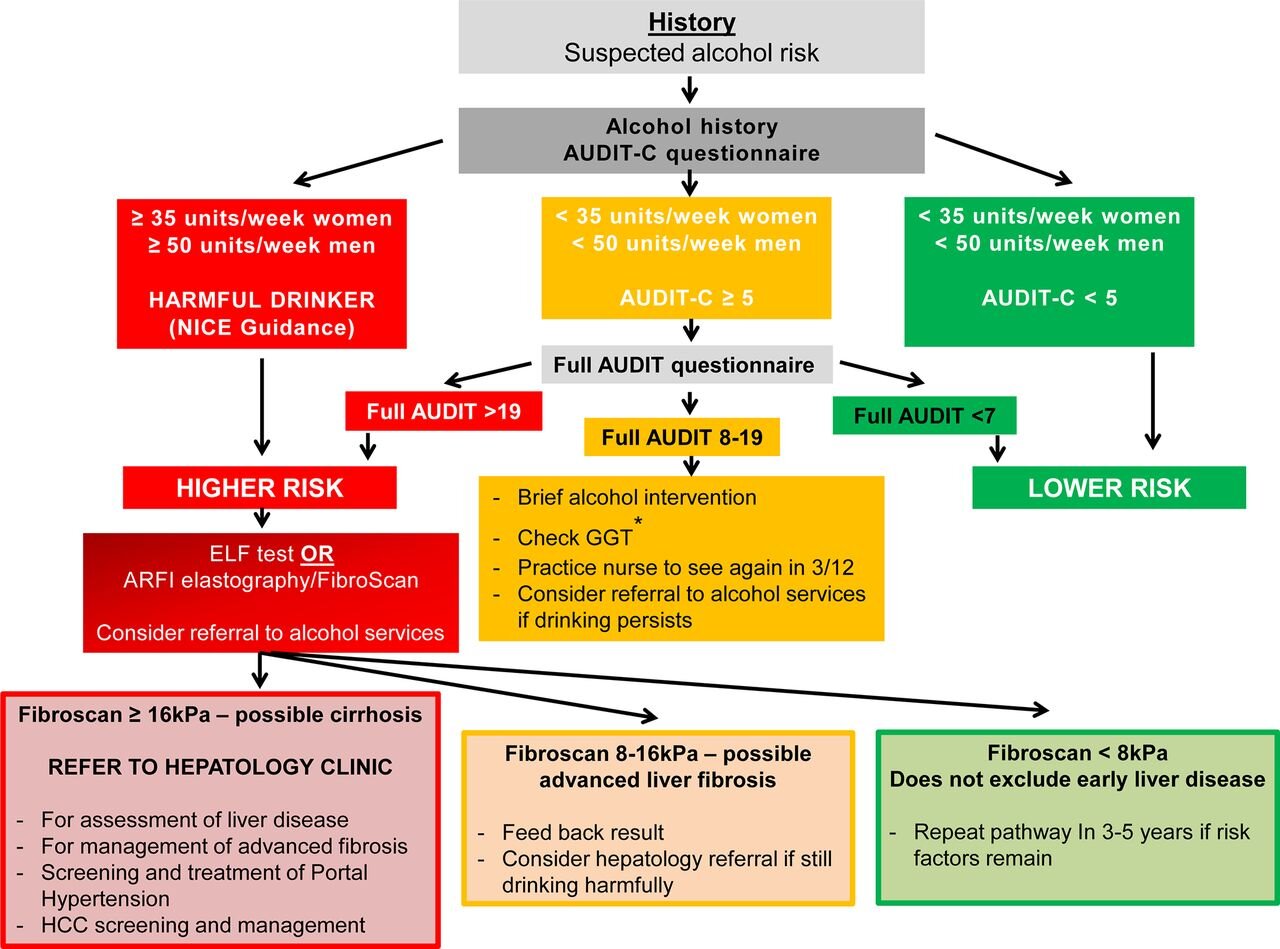
Alcohol assessment questionnaire
Alcohol Use Disorders Identification Test (AUDIT) or Fast Alcohol Screening Test (FAST) to detect excessive alcohol intake
Normal liver blood tests do not rule out advanced liver fibrosis and cirrhosis
Management
In all cases of ARLD, aim for alcohol abstinence.
However, heavy dependent drinkers should be advised to slowly reduce their alcohol intake, otherwise there is a risk of acute alcohol withdrawal, seizures, and delirium tremen.
Patients should be advised to slow the rate of reduction if they develop symptoms of withdrawal such as irritability, palpitations, sweating, nausea, and tremor.
Ideally, the alcohol reducing regimen should be supervised by an addiction specialist nurse/practitioner.Quantify alcohol consumption: AUDIT-C questionnaire
Referral to alcohol addiction services
indicated if alcohol dependent (AUDIT score of >19)
considered if AUDIT score of ≥8At level of HARMFUL DRINKER (> 50 units/week in men and >35 units/week in women) OR AUDIT>19, then undertake liver bloods tests and abdominal ultrasound and screening for advanced liver fibrosis (Fibroscan).
High alcohol consumption, but less than HARMFUL DRINKER level, AUDIT C>5, then undertake liver blood tests, abdominal ultrasound and consider screening for advanced liver fibrosis (Fibroscan), particularly if GGT>100. Implement brief alcohol intervention and consider referral to alcohol addiction services.
Regardless of whether individual is HARMFUL DRINKER or HAZARDOUS DRINKER, if there is evidence of advanced liver disease (features of cirrhosis or portal hypertension on imaging or from blood tests) and/or Fibroscan reading is >16 kPa then refer to Hepatology.
Consider referral to Hepatology if Fibroscan 8-16 kPa (possible advanced liver fibrosis) and individual is still drinking harmfully despite alcohol intervention/referral to alcohol addiction services.
The enhanced liver fibrosis (ELF) test and FIB-4 score (includes age, AST, ALT and platelets) tests have been validated for NAFLD but not validated for ARLD.
A low FIB-4 to excludes cirrhosis in NAFLD and management may continue in primary care with regular reassessment.Correct thiamine deficiency e.g. 200 mg/day or 300mg/day. Regular treatment with thiamine can help prevent thiamine deficiency and reduce the risk of alcohol related brain disease, Wernicke’s encephalopathy, and Korsakoff’s syndrome.
Nalmefene is an opioid receptor antagonist, similar to naltrexone. Patients take nalmefene on an “as required” basis before they start drinking, as the drug is believed to reduce the urge to drink by reducing the reinforcing effect of alcohol. It has been shown to reduce alcohol intake in dependent drinkers when combined with psychosocial support.
Only individuals with alcohol dependence that DO NOT have physical withdrawal symptoms, and who DO NOT require immediate detoxification are considered suitable for nalmefene.
Nalmefene SHOULD NOT BE USED be used in patients with withdrawal symptoms, those who require immediate detoxification, those with recent or current opioid use, or those who have Child-Pugh C cirrhosis. It should be used with caution in patients with mild to moderate hepatic impairment.
Hospital management of alcoholic liver cirrhosis
According to NICE, all patients with ARLD cirrhosis should be seen every six months:
Assessment of liver disease (Full blood count, Urea and electrolytes, Liver blood tests, Coagulation profile, Alpha-fetoprotein (AFP))
Calculate the Model for End Stage Liver Disease (MELD) score for people with compensated cirrhosis [4] A score of 12 indicates an increased risk of liver related complications, such as ascites, encephalopathy, and variceal haemorrhage
Examine patients for complications, such as ascites or encephalopathy
Management of advanced fibrosis
OGD screening and treatment of portal hypertension and oesophageal varices
Blood (AFP) and ultrasound screening for hepatocellular carcinoma (HCC)
Thiamine replacement
All patients with cirrhosis should have regular liver ultrasonography every six months for hepatocellular carcinoma (HCC) surveillance (1% to 2% risk of HCC per year in people with ARLD cirrhosis). The aim of surveillance is to diagnose HCC early when the tumour is small and confined to the liver, and may be suitable for a curative treatment such as radiofrequency ablation or liver resection.
OGD endoscopy is recommended at the time of diagnosis of cirrhosis, and three years after.
If moderate or large varices are identified, a non-cardioselective beta-blocker such as propranolol or carvedilol should be used to reduce the portal pressure and risk of variceal bleeding.
NICE guidelines on cirrhosis recommend endoscopic variceal band ligation for the primary prevention of bleeding for people with cirrhosis who have medium to large oesophageal varices.
Patients with cirrhosis are also at significant risk of osteoporosis, particularly of the spine, so they should have bone densitometry and a fracture risk assessment at diagnosis and every two years after, with appropriate treatment given if indicated.