Investigation of abnormal liver blood tests (LFTs)
Guidelines on the management of abnormal liver blood tests are available as an open access resource, produced by BSG (British Society of Gastroenterology), published in 2017.
Key:
ALP, alkaline phosphatase, GGT, γ-glutamyltransferase
AST, aspartate aminotransferase , ALT, alanine aminotransferase
INR, international normalised ratio
LDH, lactate dehydrogenase;
NAFLD, non-alcoholic fatty liver disease
ARLD, alcohol-related liver disease
PBC, Primary biliary cholangitis (cholestatic liver enzymes+ anti-mitochondrial Ab)
PSC, primary sclerosing cholangitis cholestatic liver enzymes ± IBD)
AIH Auto-immune hepatitis (raised IgG ± positive autoantibodies)
Haemochromatosis (raised ferritin and transferrin saturation >45%)
Key Learning
The most common causes of abnormal liver blood tests (non-alcoholic fatty liver disease, alcohol-related liver disease and hepatitis C) are frequently associated with only mild or moderate liver blood test abnormalities.
Regrettably, many of these individuals are not adequately investigated.
Therefore, patients continue to present with undiagnosed end-stage liver disease, which might have been preventable by earlier diagnosis.
Patients with abnormal liver blood tests should be considered for investigation with a liver aetiology screen irrespective of level and duration of abnormality. Abnormal refers to an analyte which is outside the laboratory reference range
Further evidence is required to establish the most cost-effective approach to identify patients with ARLD and NAFLD at risk of having advanced liver fibrosis.
Which individuals require liver blood tests
Non-specific symptoms: fatigue, nausea or anorexia
Evidence of chronic liver disease: cirrhosis, portal hypertension, liver failure, peripheral oedema, spider naevi and hepatosplenomegaly
Evidence of malignancy: jaundice, abdominal pain, weight loss, pruritus
Harmful levels of alcohol : enquire about current and past intake in average units per week, consider AUDIT C. Harmful levels of alcohol: more than 50 units/week in men and 35 units/week in women require liver bloods tests and screening using Fibroscan
Viral Hepatitis: at risk groups include people who inject drugs, migrants from high-prevalence areas, prisoners
At risk of developing liver disease:
primary biliary cholangitis worsening pruritus
primary sclerosing cholangitis pre-existing inflammatory bowel disease UC, Crohn’s
hepatotoxic drugs: amiodarone, carbamazepine, methyldopa, minocycline, macrolide antibiotics, nitrofurantoin, statins, sulfonamides, terbinafine, chlorpromazine and methotrexate
drugs causing cholestatic pattern of liver enzymes: carbamazepine, isotretinoin, methotrexate, oral contraceptives, phenobarbital, phenytoin, and valproic acid
familial liver disease: haemochromatosis or Wilson’s disease: ferritin, transferrin saturation, haemochromatosis genotype, caeruloplasmin and urinary copper.
? At risk of NAFLD because of features of the metabolic syndrome (central obesity, hypertension, diabetes/insulin resistance and dyslipidaemia)
What comprises the initial investigation for liver disease
FBC full blood count
LFTs (bilirubin, albumin, alanine aminotransferase (ALT), alkaline phosphatase (ALP), aspartate aminotransferase (AST))
GGT (γ-glutamyltransferase)
INR (if confirmed evidence of chronic liver disease)
An AST:ALT ratio of >1 and/or low platelet count suggests advanced hepatic fibrosis/cirrhosis and warrants REFERRAL
A raised GGT is associated with increased liver as well as all-cause (including cancer) mortality
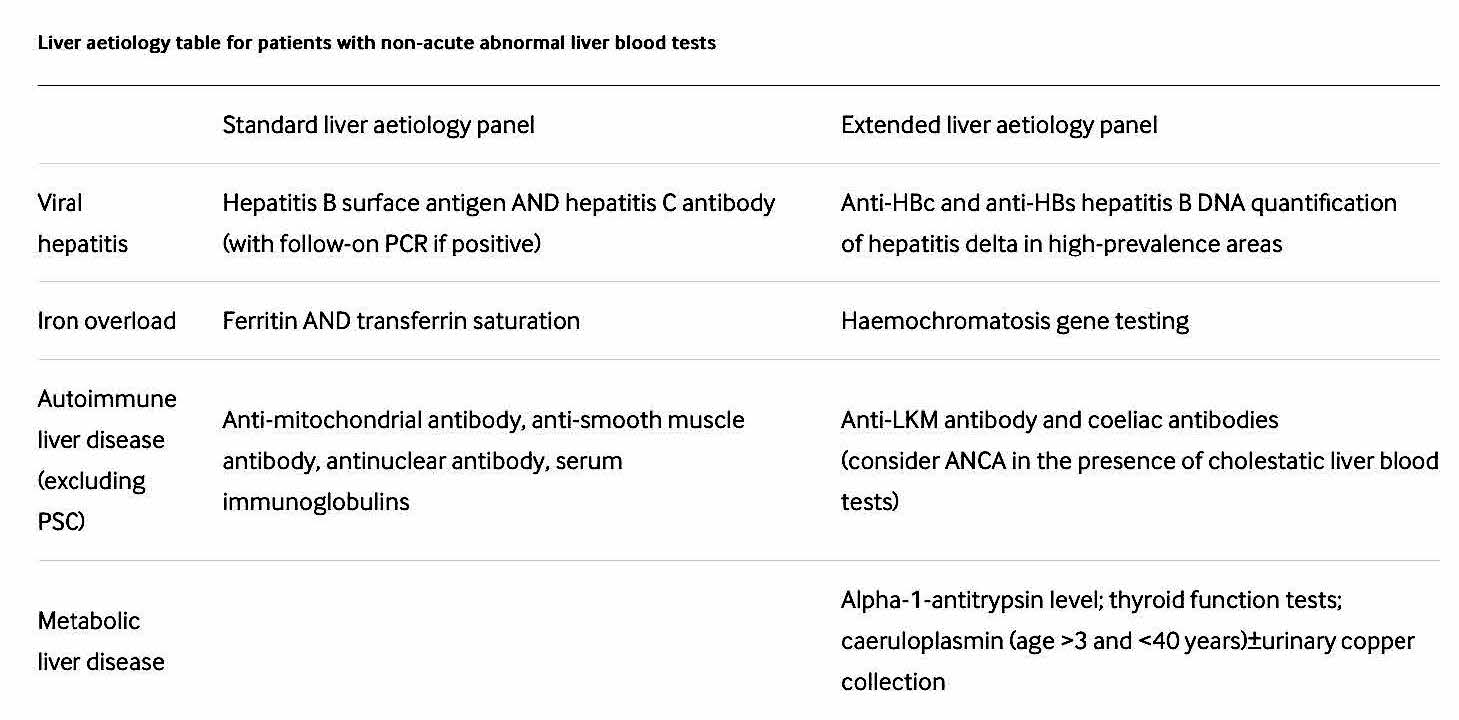
Next stage testing: liver aetiology screen (blood and abdominal ultrasound):
1. Blood tests
Viral hepatitis: Hepatitis B surface antigen, hepatitis C antibody (with follow-on polymerase chain reaction (PCR) if positive)
Iron overload: Ferritin and Transferrin saturation
Liver auto-antibodies: anti-mitochondrial antibody (PBC), anti-smooth muscle antibody, antinuclear antibody, serum immunoglobulins. And, in children, check: anti-liver kidney microsomal antibody, coeliac antibodies, alpha-1-antitrypsin level and caeruloplasmin
Others: HbA1c, Coeliac serology
2. Abdominal ultrasound scan (USS)
Features suggesting cirrhosis: irregular liver edge, nodular liver, splenomegaly, ascites, or other signs of portal hypertension
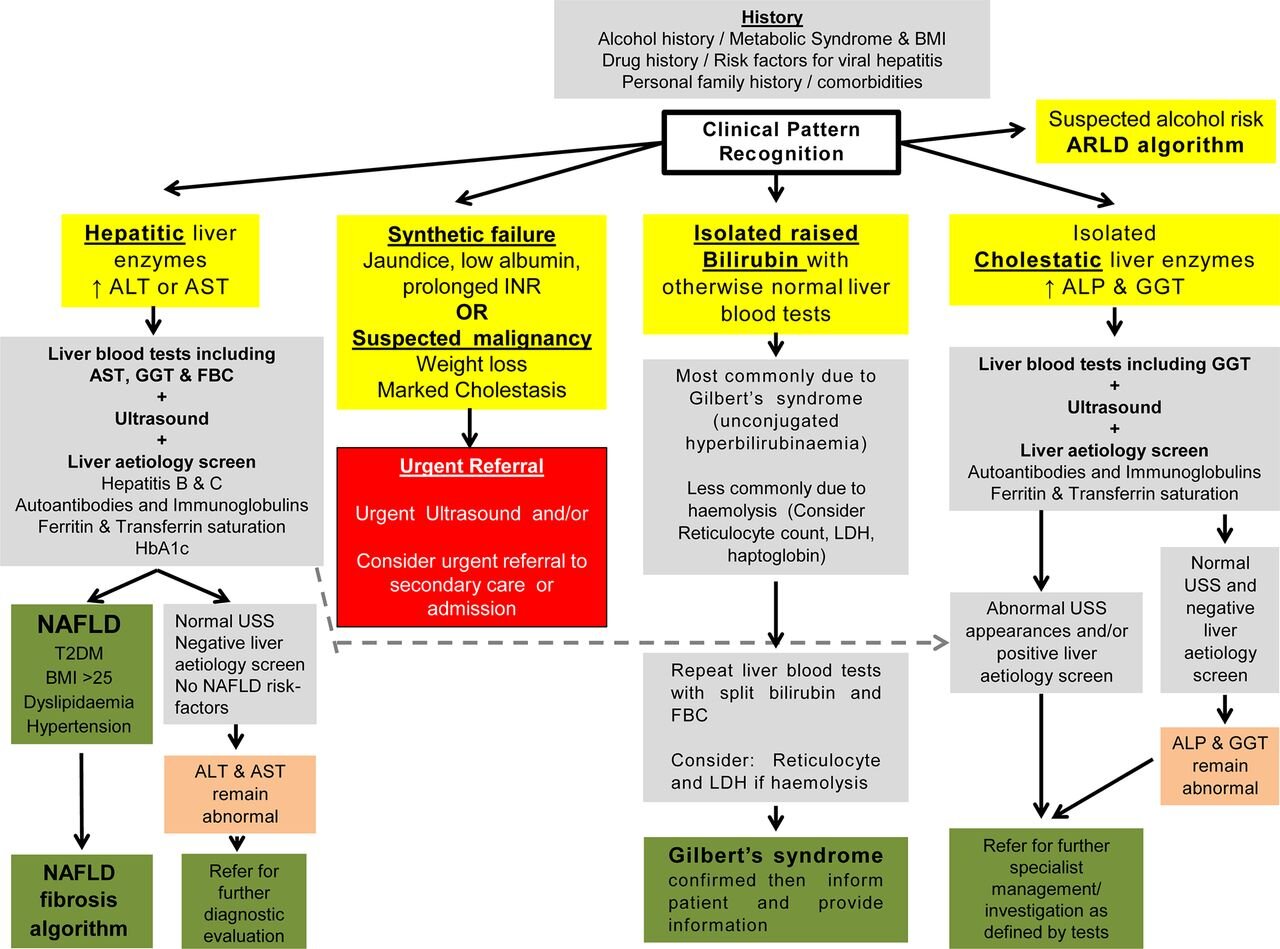
Response to abnormal liver blood tests: outcomes and pathways
URGENT REFERRAL is indicated if synthetic failure (jaundice, low albumin, prolonged INR) OR suspected malignancy (weight loss, marked cholestasis)
Undertake LIVER AETIOLOGY SCREEN (viral hepatitis, iron overload and liver auto-antibodies + Abdo USS) if abnormal ALT/AST or abnormal ALP/GGT (cholestasis)
Adults with abnormal liver blood tests, even with a negative extended liver aetiology screen and no risk factors for NAFLD, should be REFERRED for further investigation
Only if isolated raised bilirubin, with otherwise normal LFTs, then repeat a fasting test blood-if haemolysis is excluded (reticulocyte count, LDH, haptoglobin) and unconjungated hyperbilirubinaemia remains, likely diagnosis is Gilbert’s syndrome.
Haemochromatosis (raised ferritin and transferrin saturation >45%) should be distinguished from isolated elevated serum ferritin (commonly seen in alcohol excess, NAFLD and other chronic liver diseases).
A raised ferritin with normal transferrin saturation (less than 45%) and a raised mean corpuscular volume (MCV) is suggestive of ARLD
Bilirubin
Lab reports total bilirubin, which comprises unconjugated and conjugated fractions.
Bilirubin is transported to the liver in its insoluble unconjugated form, where it is converted into soluble conjugated bilirubin in order to be excreted:
Unconjugated hyperbilirubinaemia is usually due to
haemolysis (high reticulocytes/lactate dehydrogenase and low haptoglobin)
impaired conjugation (e.g. Gilbert’s syndrome; fasting sample should raise indirect component without causing anaemia)
or rare syndromes (Bil >40 μmol/L could indicate Crigler-Najjar syndrome; genetic testing needed).
Conjugated hyperbilirubinaemia is typically due to parenchymal liver disease or obstruction of the biliary system.
Gilbert's syndrome
Isolated elevated bilirubin concentration
Inherited disorder of metabolism and leads to impaired conjugation via reduced activity of the enzyme glucuronyltransferase.
Gilbert’s syndrome is not associated with liver disease or ill health
Albumin
Albumin is a protein that is produced only in the liver, hence serum serum albumin concentration is considered as a marker of the synthetic function of the liver.
Albumin concentrations are reduced in chronic liver disease, sepsis, systemic inflammatory disorders, nephrotic syndrome, malabsorption and gastrointestinal protein loss.
Prothrombin time (PT) and INR
Protein clotting factors (II, V, VII, IX and X) are made in the liver.
Significant liver injury (>70% of synthetic function), results in a reduction in clotting factor production and coagulopathy confirmed by a prolonged PT or INR.
Prolonged PT/INR occurs in other conditions that cause vitamin K deficiency (e.g fat malabsorption and chronic cholestasis).
Low platelets (thrombocytopenia)
Low platelets are an indicator of advanced liver disease.
Multiple factors culminate in a low platelet count: decreased production, splenic sequestration and increased destruction.
Alkaline phosphatase (ALP)
Alkaline phosphatase (ALP) is found in liver, bone, intestines, kidneys and white blood cells.
Increased ALP occurs with:
Bone disease e.g. metastatic bone disease and bone fractures
Cholestatic liver disease (dually-elevated ALP and GGT) e.g. primary biliary cholangitis, primary sclerosing cholangitis (PSC), biliary obstruction (stones, strictures, neoplasia) that may be intrahepatic (cholangiocarcinoma) or extrahepatic (pancreatic cancer), hepatic congestion (secondary to right-sided heart failure) and drug-induced cholestasis (e.g. carbamazepine).
Isolated ALP elevation
Isolate ALP elevation WITHOUT elevated GGT OR confirmed elevated non-hepatic isoenzyme ALP
Causes: vitamin D deficiency, rapid childhood growth, Paget’s disease and bony metastases.
AST, aspartate aminotransferase and ALT, alanine aminotransferase (hepatocyte injury/hepatitis)
ALT is considered more liver-specific since it is present in low concentrations in non-hepatic tissue
AST is present in liver, skeletal, cardiac and smooth muscle; hence elevated AST can occur with myocardial infarction or myositis.
Elevated AST and ALT occur with hepatitis, NAFLD, ARLD, autoimmune hepatitis (AIH) and drug-induced liver injury
An AST:ALT ratio of >1 and/or low platelet count suggests advanced hepatic fibrosis/cirrhosis and warrants REFERRAL
γ-Glutamyltransferase (GGT)
GGT is present in the liver, kidney, intestine, prostate and pancreas but not in bone; therefore it can be useful in confirming that an elevated ALP is of liver and not bony origin.
Elevated GGT occurs with: obesity, NAFLD, drug-induced liver injury, cholestatic liver disorders, liver metastases, and hepatic congestion secondary to heart failure.
A raised GGT is associated with increased liver mortality and all-cause (including cancer) mortality
In NAFLD a raised GGT is the most common liver enzyme abnormality, and the only liver enzyme abnormality that is independently associated with hepatic steatosis.